Why you should know the many unique harbingers of giant cell arteritis
The contents of this article are informational only and are not intended to be a substitute for professional medical advice, diagnosis, or treatment recommendations. This editorial presents the views and experiences of the author and does not reflect the opinions or recommendations of the publisher of Optometry 360.
By Christopher Kuc, OD
Giant cell arteritis (GCA) is a condition that should always be on the radar of practicing optometrists. Although its incidence is low (10-20 per 100,000),1 understanding the clinical picture that presents in those at greatest risk is paramount to saving vision in patients affected by this subtle disease. Ischemic optic neuropathy is an avoidable ocular emergency if a patient is discovered before this unfortunate endpoint. But what are some of the varying effects that GCA poses to the ocular and periocular region? In this case review, we examine 2 distinct presentations of this often-devastating type of arteritis.
Case 1
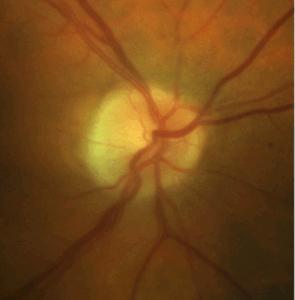
A 78-year-old white male was referred by his primary care physician for the possibility of shingles with visual symptoms. He complained of “splotches of paint” or shade in his vision, and he had recently bumped his head, which first bruised and then progressed to scabbed lesions (Figure 1), which he still described as tender to the touch. His medical history was significant for type 2 diabetes, hypertension, and basal cell carcinoma. His clinical findings were: BCVA 20/25 OD, 20/30 OS; questionable APD OS; IOP of 16 OU; and unremarkable anterior segment exam with posterior chamber IOLs OU. Upon dilation, his fundus exam is shown in Figure 2. He had a palpable temporal artery bilaterally, and blood pressure was 139/92 RAS. Stat labs were ordered, including CBC, FBS, lipid profile, ESR, CRP, platelets, Bartonella, syphilis, and Lyme.

Figure 1. Scabbed lesions that do not respect the midline.
Courtesy of Dr. Christopher Kuc

Figure 2. Disc edema OS demonstrating telangiectatic vessels.
Courtesy of Dr. Christopher Kuc
Case 2
A 79-year-old white male presented for evaluation of horizontal diplopia, which had started intermittently 5 days prior and became constant 3 days ago. He was admitted overnight to the hospital, where a CT of the head with and without contrast was performed along with an MRI without contrast. Both were negative. Extensive bloodwork, including myasthenia gravis autoantibody panel, was performed. All labs were unremarkable. His medical history was significant for hypertension and hypercholesterolemia, which likely led the caring physicians to believe this was an ischemic cranial nerve 6 palsy.
Upon further questioning, his review of systems was notable for weight loss, which he attributed to decreased appetite and night sweats over the past 6 months. His clinical findings were: BCVA 20/30- OD, 20/25- OS; and constant right esotropia, which measured 20 PD on gaze right, 16 PD in primary, and 12 PD on gaze left with limited abduction OD on versions (Figure 3). No APD was noted. Anterior segment exam revealed normal ocular surface and anterior chamber with IOP 12 OU and 2+ nuclear sclerotic cataracts. Posterior segment exam was unremarkable. After requesting labs from his hospital stay and noting the absence of erythrocyte sedimentation rate, C-reactive protein, and platelets, stat labs were ordered following his office visit.

Figure 3. Example of restricted abduction OD on gaze R.
Courtesy of Dr. Christopher Kuc
Discussion
GCA is an autoimmune vasculitis found almost exclusively in individuals older than 50, with peak incidence between the ages of 70 and 79 years. It is most common in patients of Northern European descent and affects women to men at a ratio of up to 3:1.2 Cranial GCA can affect medium-sized vessels of the head and neck. In the chest, aortic dissection and aneurysm are possible outcomes for those suffering from damage to large-sized vessels.
When considering cranial GCA, the most common vessel affected is the temporal artery, for which the condition is also sometimes named for: “temporal arteritis.” Although ischemic optic neuropathy is probably the most notorious outcome affecting the eye, there are a number of ocular and periocular complications that may present clinically with the underlying disease due to the pathway of arteries affected. For any patient older than 50 who has a recent onset headache, especially with scalp tenderness, GCA should be on the list of differential diagnoses. Further questioning regarding commonly associated symptoms should include jaw claudication, fever, malaise, anorexia, night sweats, and arthralgia (especially neck or shoulder, as there is a strong association with polymyalgia rheumatica).3 Ocular symptoms may include amaurosis fugax, diplopia, or eye pain.
The arteries affected by GCA undergo inflammation and disruption of the internal elastic lamina with intimal hyperplasia, which causes narrowing of the vessel lumen (Figure 4).4 When examining the pathway of the ischemia this induces, understanding the anatomy can lead to logical conclusions of clinical findings. Common ocular sequela of GCA is arteritic ischemic optic neuropathy, central retinal artery occlusion, cotton wool spots, choroidal infarcts, diplopia/EOM disorders, and anterior segment ischemia.5

Figure 4. Resolved lesions.
Courtesy of Dr. Christopher Kuc
Update on Patient 1
The patient’s lab work came back as positive for ESR 92 mm/Hr, CRP 121 mg/L, and 440k/mL. Although his early nerve ischemia OS was the driving factor for his workup, his scabbed lesions were actually related to GCA in the form of scalp necrosis. The pathway for involvement involves the supraorbital and supratrochlear arteries, which are direct branches of the ophthalmic artery that is commonly involved in GCA (Figure 5). Although Herpes zoster has been implicated in some cases of GCA, this was not typical of a zoster lesion, which would respect the midline. A temporal artery biopsy was obtained following positive labs, and the patient was started on 60 mg of oral prednisone daily. His lesions resolved slowly with treatment (Figure 6), and his optic disc edema OS resolved prior to any further insult to the optic nerve.

Figure 5. Narrowed lumen of an artery with GCA.
Source: Wantanabe R, Hashimoto M. Pathogenic role of monocytes/macrophages in large vessel vasculitis. Front Immunol. 2022;13:859502. doi:10.3389/fimmu.2022.859502

Figure 6. Supraorbital and supratrochlear arteries, direct branches of the ophthalmic artery. Source: https://plasticsurgerykey.com/10-facial-danger-zone-1-glabellar-region/#c010_f003
Update on Patient 2
His levels were elevated at ESR 63 mm/Hr, CRP 38.6 mg/L, and 390K/mL. His isolated right sixth nerve palsy was a direct result of GCA. He was started on 60 mg of oral prednisone, and temporal artery biopsy was subsequently ordered, which returned positive. Upon treatment, his horizontal diplopia resolved within a few weeks. In cases of apparent isolated sixth nerve palsy, the ischemia induces damage to the nerve. This can be direct branches of the ophthalmic artery or the inferolateral trunk of the internal carotid artery (Figure 7).

Figure 7. Branches of the ophthalmic artery.
Courtesy of Netter FH. Atlas of Human Anatomy, 2nd Edition. 1997.
Conclusion
Many patients with GCA will need long-term therapy with prednisone, sometimes over the course of years or a lifetime. This requires some clever medical monitoring, especially for patients with diabetes. One alternative to oral prednisone is an IL-6 receptor antagonist such as tocilizumab.
Understanding the artery distribution affected by GCA can lead to diagnoses that fall outside of ischemic optic neuropathy. As eye care providers, it is important to be aware of the many unique harbingers of GCA.
Christopher Kuc, OD, is the Medical Director of Medical Optometry America – Newtown Square. Disclosures: Dr. Kuc is a speaker for Bausch + Lomb, consultant for Zeiss and Tarsus, and shareholder in VisionLock.
References
- Li KJ, Semenov D, Turk M, Pope J. A meta-analysis of the epidemiology of giant cell arteritis across time and space. Arthritis Res Ther. 2021;23(1):82. doi:10.1186/s13075-021-02450-w
- Ameer MA, Vaqar S, Khazaeni B. Giant cell arteritis (temporal arteritis) [Updated 2024 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. https://www.ncbi.nlm.nih.gov/books/NBK459376/
- Awisat A, Keret S, Silawy A, et al. Giant cell arteritis: state of the art in diagnosis, monitoring, and treatment. Rambam Maimonides Med J. 2023;14(2):e0009. doi:10.5041/RMMJ.10496
- Héron E, Sedira N, Dahia O, Jamart C. Ocular complications of giant cell arteritis: an acute therapeutic emergency. J Clin Med. 2022;11(7):1997. doi:10.3390/jcm11071997
- Hayreh SS, Podhajsky PA, Zimmerman B. Ocular manifestations of giant cell arteritis. Am J Ophthalmol. 1998;125(4):509-520. doi:10.1016/s0002-9394(99)80192-5
Additional source: Anatomy of the periorbital region.

Contact Info
Grandin Library Building
Six Leigh Street
Clinton, New Jersey 08809